Nursing Chart Audits
Nursing Chart Audits - Comments from nurses on the chart audit initially, some nurses resisted the chart. Web this study showed the significance of documentation audit in ensuring completeness of patients’ records, the role of nurses in audits and the opportunity audits provide to compare documentation guidelines with the. Part of the other analytical, diagnostic and therapeutic techniques and equipment commons. Web what is a nurse auditor? Web the duties of an rn chart auditor are to review medical records for accuracy, quality assurance, or billing and insurance purposes. The steps in this article will help you initiate your audit and see you through the entire process from identifying audit targets to implementing a plan to prevent the discovered deficiencies. 1 2 audit and feedback aim to improve patient care by reviewing clinical performance against explicit standards and directing action towards areas not meeting those standards. Creating an effective nursing audit checklist is essential for maintaining the highest standards of patient care and ensuring compliance with healthcare regulations. Percentage of charts with complete documentation. How should feedback be provided? The steps in this article will help you initiate your audit and see you through the entire process from identifying audit targets to implementing a plan to prevent the discovered deficiencies. A chart audit is an examination of medical records (electronic and/or hard copy), to determine what has been done, and see if it can be done better. A pre. University of new hampshire, durham. Creating an effective nursing audit checklist is essential for maintaining the highest standards of patient care and ensuring compliance with healthcare regulations. University of san francisco, [email protected]. Web the goal of this chart audit was not only to assess the completeness of nursing documentation on the unit but also to review the nursing practice, standards. Last updated on march 26, 2024 by ossian muscad. 1 2 audit and feedback aim to improve patient care by reviewing clinical performance against explicit standards and directing action towards areas not meeting those standards. Web healthcare systems face challenges in tackling variations in patient care and outcomes. This project assessed nurses' documentation skills and consistency between prescribed care and. 3 it is a widely used foundational component of quality improvement, included. Web the goal of this chart audit was not only to assess the completeness of nursing documentation on the unit but also to review the nursing practice, standards of care, and consistency of treatment provided. This project assessed nurses' documentation skills and consistency between prescribed care and care. University of new hampshire, durham. Last updated on march 26, 2024 by ossian muscad. Meeting joint commission compliance by improving the chart audit process. University of san francisco, [email protected]. The steps in this article will help you initiate your audit and see you through the entire process from identifying audit targets to implementing a plan to prevent the discovered deficiencies. During chart auditing, several issues were identified. 1 2 audit and feedback aim to improve patient care by reviewing clinical performance against explicit standards and directing action towards areas not meeting those standards. Follow this and additional works at: Web nursing audit is the process of analyzing data about the nursing process of patient outcomes to evaluate the effectiveness of. Web the duties of an rn chart auditor are to review medical records for accuracy, quality assurance, or billing and insurance purposes. Web the audits used in the area of improving healthcare can roughly be divided into: Your responsibilities include assessing medical records to decide whether there is a valid reason for treatment or denial of care and ensure that. Your responsibilities include assessing medical records to decide whether there is a valid reason for treatment or denial of care and ensure that the quality of patient care abides by health care policies and. How should feedback be provided? Web the goal of this chart audit was not only to assess the completeness of nursing documentation on the unit but. Percentage of charts with complete documentation. 1 2 audit and feedback aim to improve patient care by reviewing clinical performance against explicit standards and directing action towards areas not meeting those standards. Your responsibilities include assessing medical records to decide whether there is a valid reason for treatment or denial of care and ensure that the quality of patient care. Accreditation, certification, external peer reviews); Creating an effective nursing audit checklist is essential for maintaining the highest standards of patient care and ensuring compliance with healthcare regulations. This project assessed nurses' documentation skills and consistency between prescribed care and care provided to patients. How should feedback be provided? Web this study showed the significance of documentation audit in ensuring completeness. Web run charts are a good way to aggregate audit data and share it at the unit or hospital level. Web chart audit tool on nursing assessment and device selection for vascular access and patient outcomes november 2006 5 implementation of recommendations in the bpg. Web internal audits are those which are performed within the organization. Web this study showed the significance of documentation audit in ensuring completeness of patients’ records, the role of nurses in audits and the opportunity audits provide to compare documentation guidelines with the. Last updated on march 26, 2024 by ossian muscad. University of new hampshire, durham. (2) internal audits, often in preparation for an external audit; 1 2 audit and feedback aim to improve patient care by reviewing clinical performance against explicit standards and directing action towards areas not meeting those standards. A nursing audit consists of collecting information from nursing reports, medical notes and other patient care records to help assess the quality of care. Follow this and additional works at: How should feedback be provided? Web what is a chart audit? 3 it is a widely used foundational component of quality improvement, included. One day a provider in the sleepytown community health center (schc) sees several patients complaining of prolonged cough. Personal feedback on chart audits on request. This project assessed nurses' documentation skills and consistency between prescribed care and care provided to patients.Medical Records Audit Checklist PDF Surgery Patient

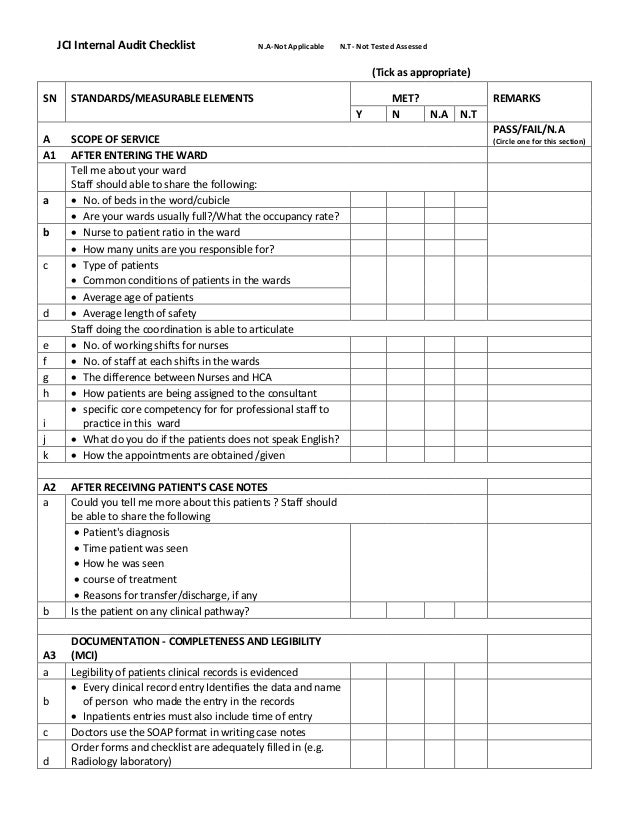
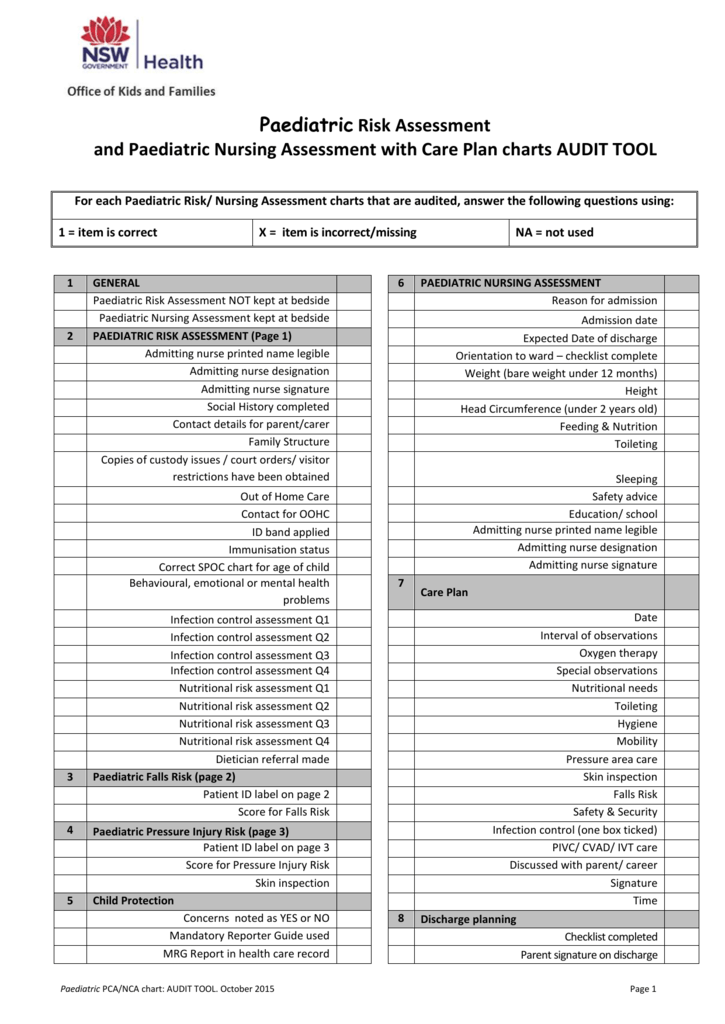
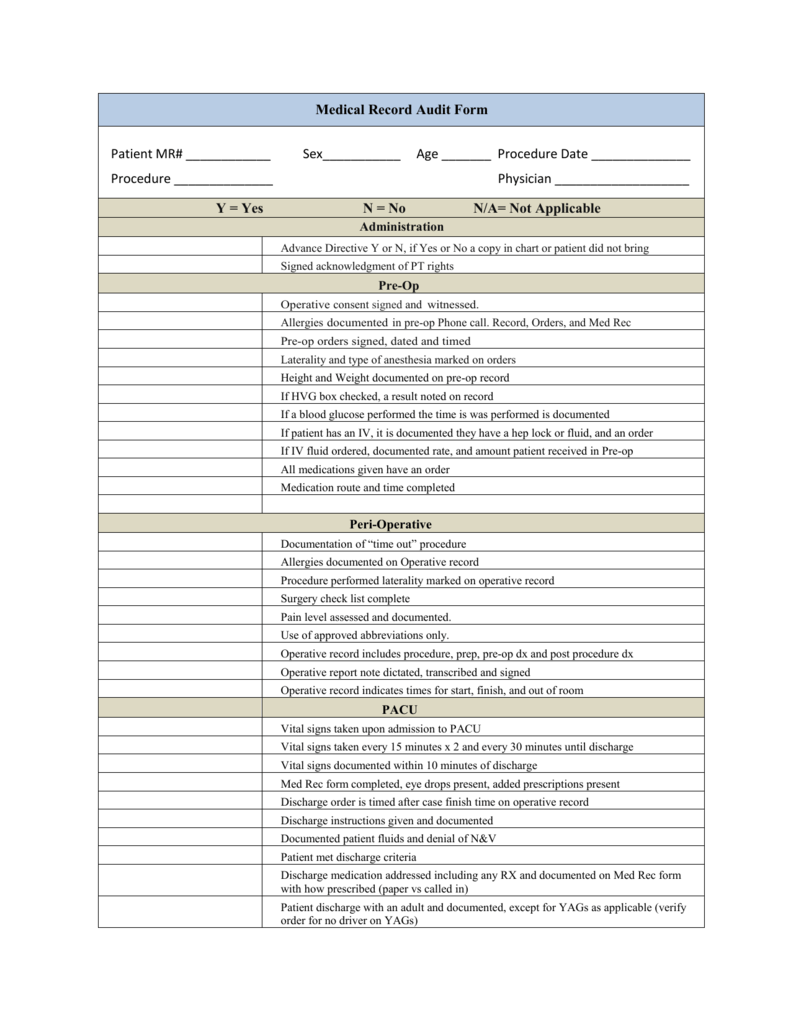
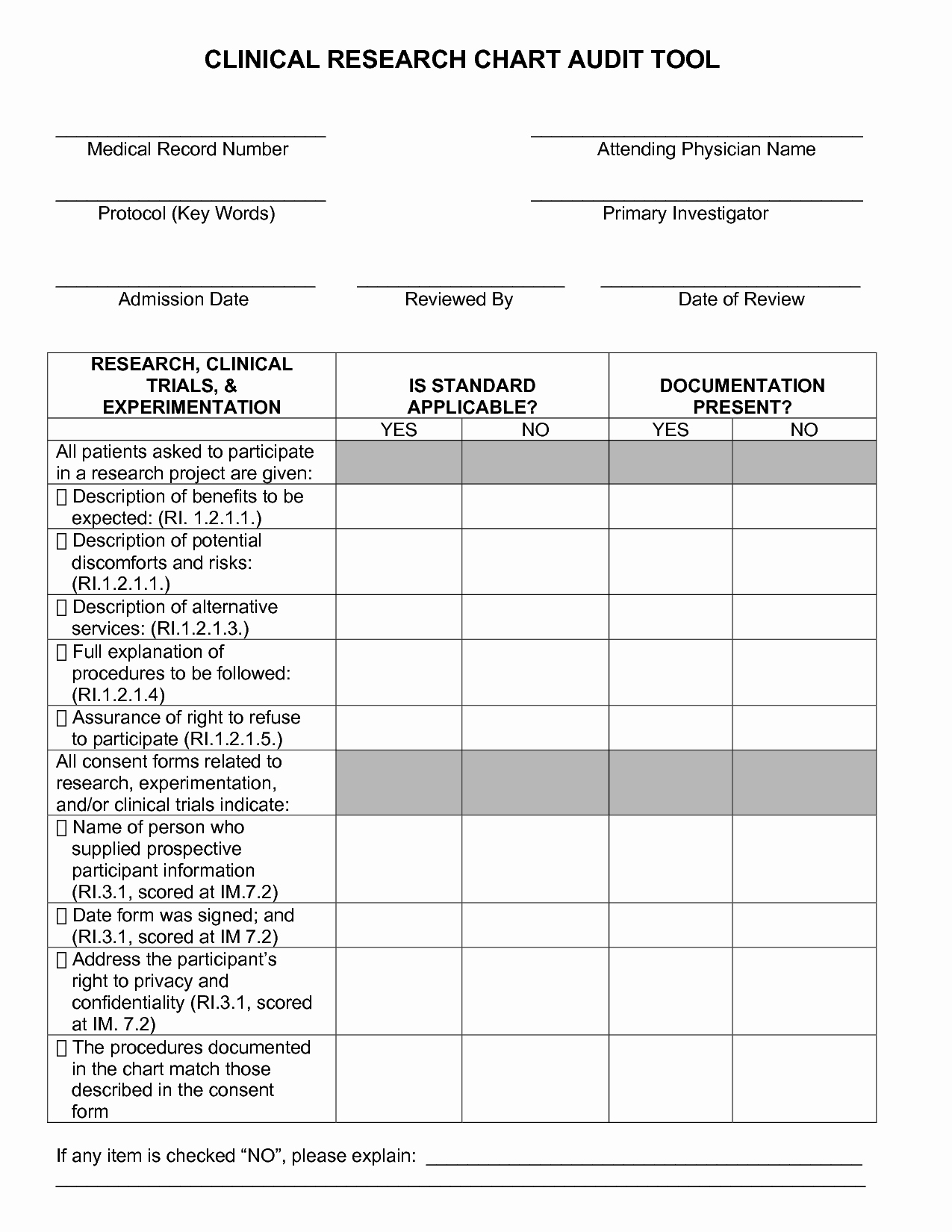
the record checklist and audit form is shown

(PDF) Nursing audit as a method for developing nursing care and

Printable Medical Chart Audit Template

Medical Chart Audit Template
Medical Chart Audit Template For Your Needs
Chart Audit PDF Major Trauma Patient
Nurse Chart Audit Templates
Nursing Chart Audit Tool Template
Nursing Chart Audit Tool Template
The Steps In This Article Will Help You Initiate Your Audit And See You Through The Entire Process From Identifying Audit Targets To Implementing A Plan To Prevent The Discovered Deficiencies.
University Of San Francisco, [email protected].
The Audits Most Frequently Used In Quality Control Include Outcome, Process And Structure Audits.
Web The Duties Of An Rn Chart Auditor Are To Review Medical Records For Accuracy, Quality Assurance, Or Billing And Insurance Purposes.
Related Post:

