Claims Adjudication Process Flow Chart
Claims Adjudication Process Flow Chart - This file helps to understand the part of us healthcare medical billing concept. The claims flow is schematically depicted by the following figure: Web it is important to know the different steps of the claim adjudication in order to understand how the insurance company determines how claims are paid, rejected or denied. This process includes steps that handle the. Streamlined operations with fewer human errors. Web claim adjudication process flowchart. The claims flow is described in three levels of detail. Less staff time tied up in claims adjudication. This process includes steps that handle the following aspects: Collecting and analyzing claim data, calculating reimbursements, and handling client complaints. This ppt set explains the claims procedure and is an essential resource for policyholders and insurance experts. This template efficiently divides the procedure into three crucial steps: Web the adjudication process is an embedded workflow within oracle health insurance claim adjudication. If respondent lodges adjudication response, must lodge response within 5 business days from receiving application or 2 business days. The first step in the embedded flow is for the application to accept the submitted claim. Figures (3) abstract and figures. Harness the power of automation. Web claim adjudication process flowchart. Adjudication made easier with a clearinghouse. Web mirra's claims adjudication solution is an advanced system designed to streamline and digitize the healthcare claims management process. Less staff time tied up in claims adjudication. Web the adjudication process is an embedded workflow within claims. This process includes steps that handle the following aspects: This ppt set explains the claims procedure and is an essential resource for policyholders. Although the specific flowchart may vary depending on the insurance payer, it generally includes the following stages: The adjudication process is an embedded workflow within claims. Web the medical claims adjudication flow chart is optimized through the electronic submission of claims, wherein automation solutions can create, verify, and submit claims electronically. How does a claim get accepted or rejected? How. This erases the need for manual paperwork. If respondent lodges adjudication response, must lodge response within 5 business days from receiving application or 2 business days from receiving notice of adjudicator acceptance, whichever is later. Web the adjudication process is an embedded workflow within oracle health insurance claim adjudication. The council for affordable quality healthcare (caqh) estimates that switching to. This process includes steps that handle the following aspects: Accessibility is increased through electronic documentation and records. Less staff time tied up in claims adjudication. Steps involved in the claim adjudication process. Insurance claims data flow diagram. It consists of a number of configurable steps, each of which has a specific purpose. Web ama flow that claim submission processing adjudication and payment. Health economists analyzing a single payer system don't account for enough of the savings derived from the. This file helps to understand the part of us healthcare medical billing concept. Web the adjudication process is. Web based on the claims adjudication process, the insurance company or payer determines the reimbursement amount. Web adjudication response from respondent. Web it is important to know the different steps of the claim adjudication in order to understand how the insurance company determines how claims are paid, rejected or denied. The claim adjudication process involves a flowchart of steps that. It consists of a number of configurable steps, each of which has a specific purpose. The claims adjudication workflow consists of six main steps: If respondent lodges adjudication response, must lodge response within 5 business days from receiving application or 2 business days from receiving notice of adjudicator acceptance, whichever is later. The first step in the embedded flow is. How does a claim get accepted or rejected? Health economists analyzing a single payer system don't account for enough of the savings derived from the. Web the medical claims adjudication flow chart is optimized through the electronic submission of claims, wherein automation solutions can create, verify, and submit claims electronically. This process includes steps that handle the. Web claims adjudication. This process includes steps that handle the following aspects: The claim adjudication process involves a flowchart of steps that ensure a thorough review and determination of the appropriate payment for a claim. Some of the benefits of automating healthcare claims management include: Web the adjudication flow is schematically depicted by the following figure: Web it is important to know the different steps of the claim adjudication in order to understand how the insurance company determines how claims are paid, rejected or denied. Collecting and analyzing claim data, calculating reimbursements, and handling client complaints. If respondent lodges adjudication response, must lodge response within 5 business days from receiving application or 2 business days from receiving notice of adjudicator acceptance, whichever is later. The claims flow is described in three levels of detail. The claims flow is schematically depicted by the following figure: This erases the need for manual paperwork. This guide clarifies the steps in the ohi claims adjudication process. This file helps to understand the part of us healthcare medical billing concept. It consists of a number of configurable steps, each of which has a specific purpose. Claims are an intricate and complicated process deemed prerequisite in seeking health care. The council for affordable quality healthcare (caqh) estimates that switching to electronic claims submission can save the healthcare industry $1.7 billion (about $5 per person in the us) yearly compared to manual processing. Web based on the claims adjudication process, the insurance company or payer determines the reimbursement amount.
Maximizing Returns on Your Claims AutoAdjudication Efforts A Stepby
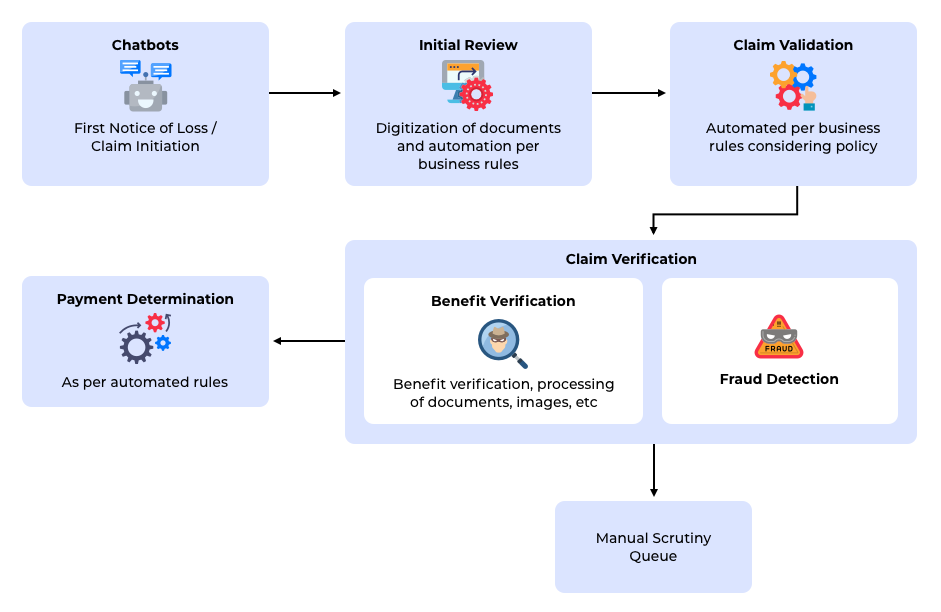
Automating Insurance Claim Adjudication
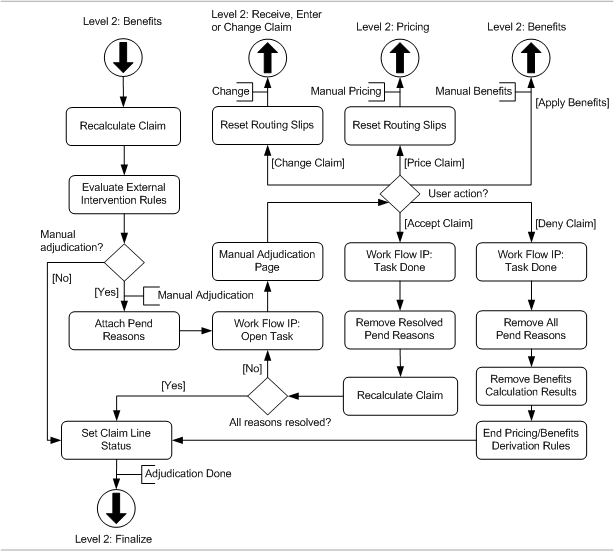
Adjudication Oracle Health Insurance Claims Adjudication and Pricing

Victoria Security of Payment & Adjudication Process
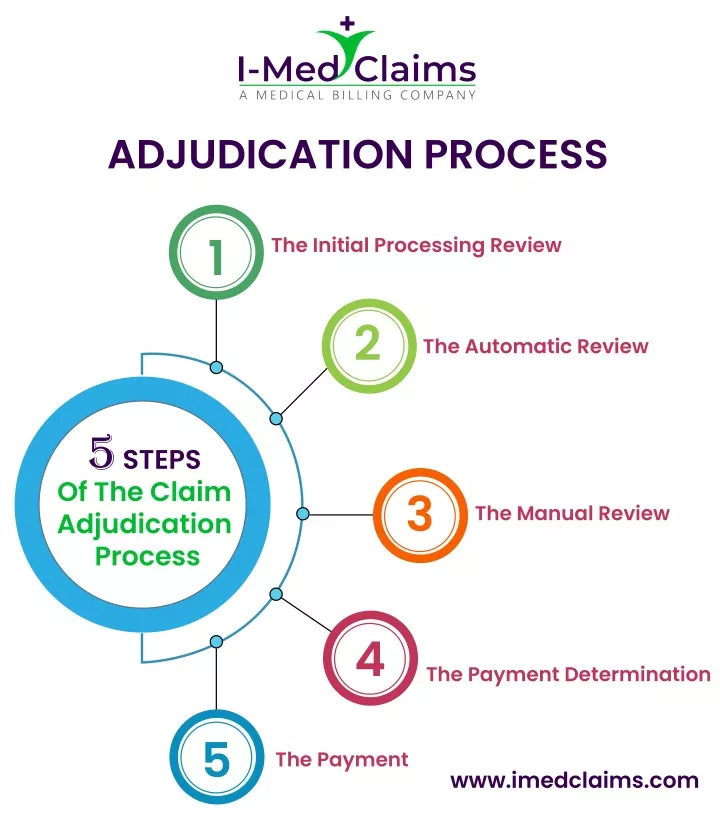
PPT 5 Steps of adjudication claim process PowerPoint Presentation

Process of adjudicating claims
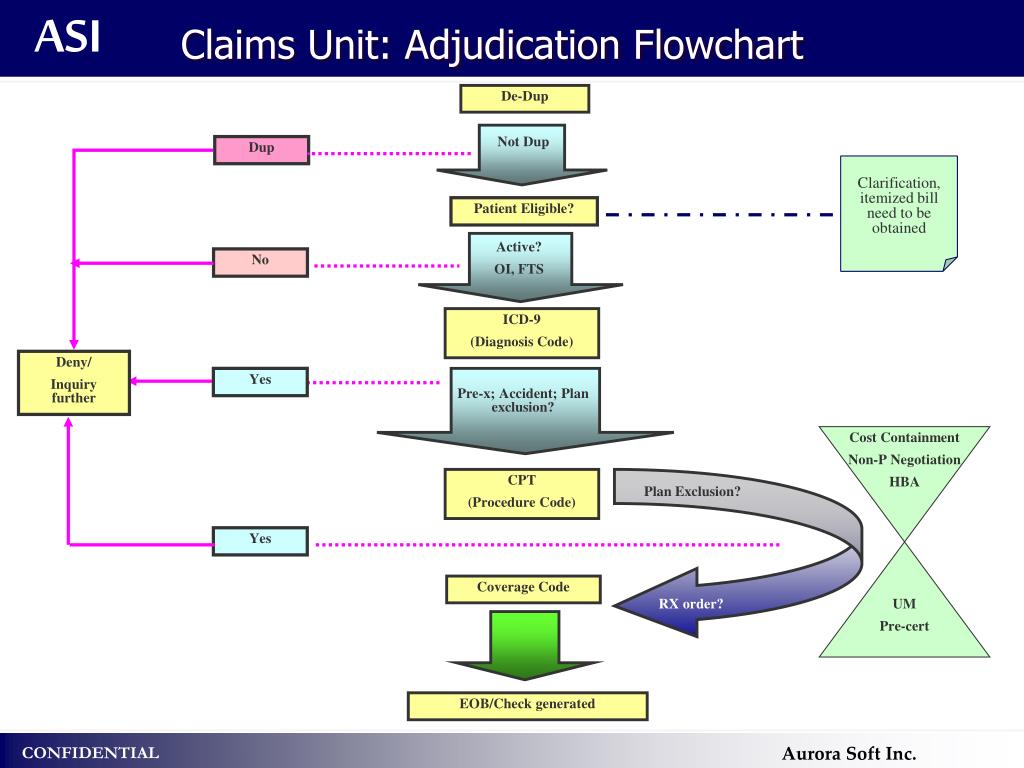
PPT Operations PowerPoint Presentation, free download ID5020714

The UI Claims Adjudication Process Department of Labor
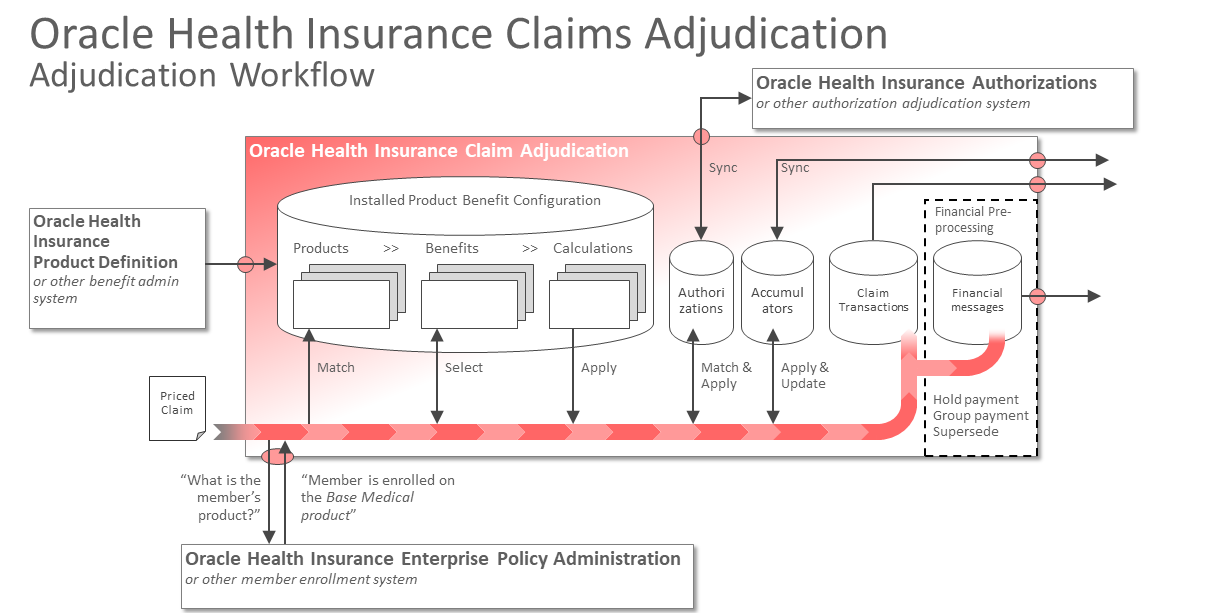
Adjudication Workflow Oracle Health Insurance Claims Adjudication

Healthcare IT EMR PMS Claims adjudication and payment
This Process Includes Steps That Handle The.
Web The Medical Claims Adjudication Flow Chart Is Optimized Through The Electronic Submission Of Claims, Wherein Automation Solutions Can Create, Verify, And Submit Claims Electronically.
It Consists Of A Number Of Configurable Steps, Each Of Which Has A Specific Purpose.
How Does A Claim Get Accepted Or Rejected?
Related Post: